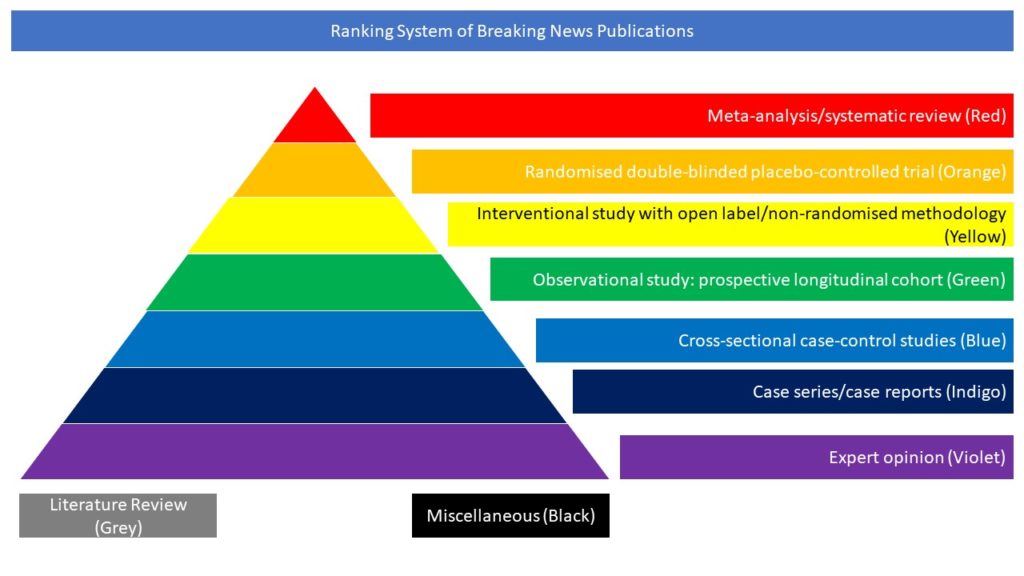
Meta-analysis/systematic review (Red)
Read on for our highlighted selection of Covid-related meta-analyses and systemic reviews from the scientific press for July 2022:
Prognostic indicators and outcomes of hospitalised COVID-19 patients with neurological disease: An individual patient data meta-analysis
Neurological COVID-19 disease has been reported widely, but published studies often lack information on neurological outcomes and prognostic risk factors. In this article the authors aimed to describe the spectrum of neurological disease in hospitalized COVID-19 patients; characterize clinical outcomes; and investigate factors associated with a poor outcome. They conducted an individual patient data (IPD) meta-analysis of hospitalized patients with neurological COVID-19 disease, using standard case definitions. They invited authors of studies from the first pandemic wave, plus clinicians in the Global COVID-Neuro Network with unpublished data, to contribute. Features associated with poor outcome (moderate to severe disability or death, 3 to 6 on the modified Rankin Scale) were analyzed using multivariable models. 83 studies (31 unpublished) were included providing IPD for 1979 patients with COVID-19 and acute new-onset neurological disease. Encephalopathy (978 [49%] patients) and cerebrovascular events (506 [26%]) were the most common diagnoses. Respiratory and systemic symptoms preceded neurological features in 93% of patients; one third developed neurological disease after hospital admission. A poor outcome was more common in patients with cerebrovascular events (76% [95% CI 67-82]), than encephalopathy (54% [42-65]). Intensive care use was high (38% [35-41]) overall, and also greater in the cerebrovascular patients. In the cerebrovascular, but not encephalopathic patients, risk factors for poor outcome included breathlessness on admission and elevated D-dimer. Overall, 30-day mortality was 30% [27-32]. The hazard of death was comparatively lower for patients in the WHO European region. Neurological COVID-19 disease poses a considerable burden in terms of disease outcomes and use of hospital resources from prolonged intensive care and inpatient admission; preliminary data suggest these may differ according to WHO regions and country income levels. The different risk factors for encephalopathy and stroke suggest different disease mechanisms which may be amenable to intervention, especially in those who develop neurological symptoms after hospital admission.
Singh B, Lant S, Cividini S, Brain Infections Global COVID-Neuro Network Study Group, Tudur Smith C, Solomon T. Prognostic indicators and outcomes of hospitalised COVID-19 patients with neurological disease: An individual patient data meta-analysis. PLoS One. 2022 Jun 2;17(6):e0263595. doi: 10.1371/journal.pone.0263595.