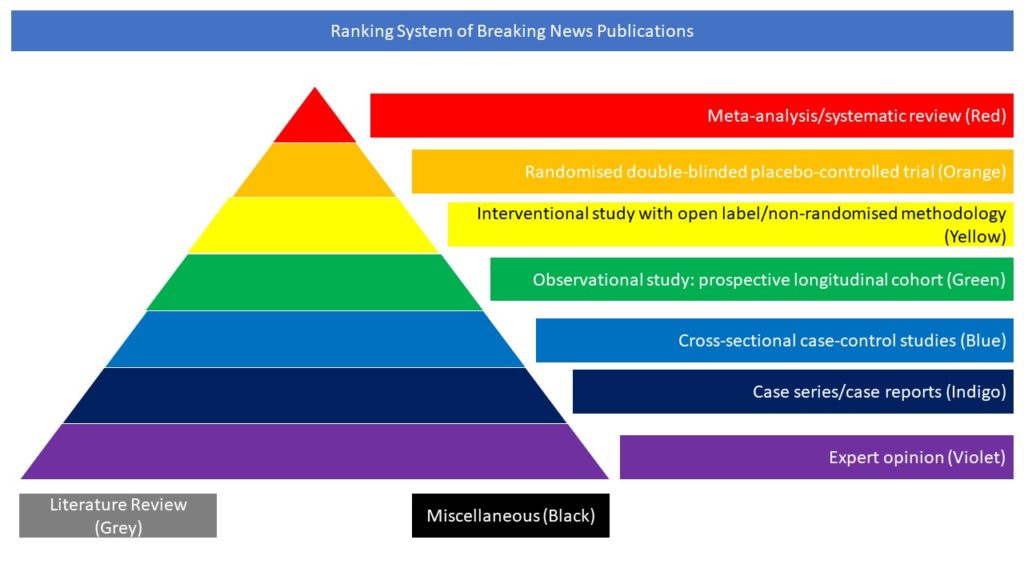
Cross-sectional case-control studies (Blue)
Acute ischaemic stroke may occur in patients with COVID-19, but risk factors, in-hospital events, and outcomes are not well studied in large cohorts. In this article, the authors identified risk factors, comorbidities, and outcomes in patients with COVID-19 with or without acute ischaemic stroke and compared with patients without COVID-19 and acute ischaemic stroke. They analyzed the data from 54 health care facilities using the Cerner deidentified COVID-19 dataset. The dataset included patients with an emergency department or inpatient encounter with discharge diagnoses codes that could be associated to suspicion of/exposure to COVID-19 or confirmed COVID-19. A total of 103 (1.3%) patients developed acute ischaemic stroke among 8163 patients with COVID-19. Among all patients with COVID-19, the proportion of patients with hypertension, diabetes, hyperlipidemia, atrial fibrillation, and congestive heart failure was significantly higher among those with acute ischaemic stroke. Acute ischaemic stroke was associated with discharge to destination other than home or death (relative risk, 2.1 [95% CI, 1.6-2.4]; P<0.0001) after adjusting for potential confounders. A total of 199 (1.0%) patients developed acute ischaemic stroke among 19 513 patients without COVID-19. Among all ischaemic stroke patients, COVID-19 was associated with discharge to destination other than home or death (relative risk, 1.2 [95% CI, 1.0-1.3]; P=0.03) after adjusting for potential confounders. The authors concluded that acute ischaemic stroke was infrequent in patients with COVID-19 and usually occurred in the presence of other cardiovascular risk factors. The risk of discharge to destination other than home or death increased 2-fold with occurrence of acute ischaemic stroke in patients with COVID-19.
DOI: 10.1161/STROKEAHA.120.031786